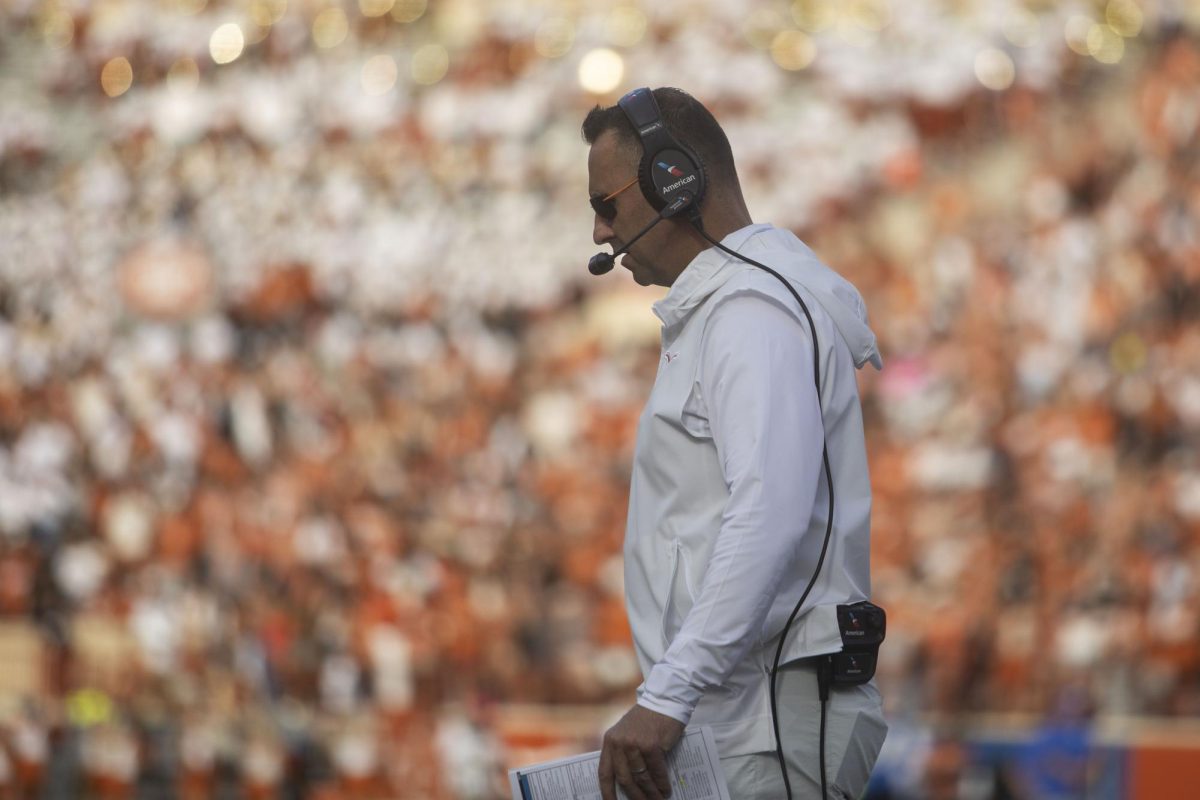
When junior quarterback David Ash took a hit in the fourth quarter against BYU on Sept. 7, no one thought anything of it. It wasn’t a vicious hit or one that rang his bell.
The training staff was unsure of the exact nature of the injury; the official injury report following the next week’s game against Ole Miss phrased his injury as head/right shoulder.
“[A concussion is] an invisible injury,” said Kenneth Locker, a prominent athletic trainer in North Texas with 20 years of concussion experience. “It happens and no one can see a change in the physical appearance of the person.”
After sitting out a blowout loss to the Rebels, Texas brought him back in for the first conference game against Kansas State just two weeks after the original injury.
He didn’t make it past halftime and hasn’t played a snap since. More than two months and seven games later, the Texas medical staff declared him finished for the season on Nov. 25.
The last few years have seen momentum in concussion awareness, ranging from high-profile documentaries such as “League of Denial” to rule changes implemented by the NFL and FBS that have attempted to curtail concussions. Ash’s injury is far from the only example in sports of career-threatening concussions: The NCAA estimates somewhere between 1.6 million and 3.8 million incidents occur in collegiate sports each year. Despite NCAA effort to develop a comprehensive protocol, concussion rates held steady between 2.2 to 3.8 percent from 2004-12, according to the NCAA injury surveillance program. The story of concussions and football are not just about the athletes who play the game, but the way institutions and governing agencies deal with them.
The NCAA mandates four steps in its handbook on how to deal with concussions. The process is outlined in a way to leave the bulk of the plans up to the discretion of each university.
For example, the handbook states that players are allowed to return to play after receiving permission from “a health care professional with experience in evaluation for concussion.”
The ability to return to play doesn’t require passing a standardized, nationally accepted test. It’s left to the discretion of the professionals on the sideline, most of whom are employed by the University. Ambiguity surrounds this injury, which is inherently difficult to diagnose on the sideline.
Concussions aren’t just head injuries — they are injuries to the brain, which the NCAA handbook defines as “a brain injury that may be caused by a blow to the head, face, neck or elsewhere on the body with an ‘impulsive’ force transmitted to the head.”
But Locker phrases it differently, calling them the most dangerous injuries in sports today.
“Concussions are from the shaking of the brain,” Locker said. “Not just head injuries.”
Repeated trauma before a full recovery worsens the issue, increasing the likelihood of long-term problems.
“If they sustain head trauma or concussions in their late teens and early 20s, the window for repetitive injury is lengthened,” Robert Glatter, an emergency medicine physician at Lenox Hill Hospital in New York City, told HealthDay in July 2012. “The long-term complications of repetitive head trauma can have lasting effects on younger athletes into their adult years.”
Long-term effects include brain swelling, sleeping problems, migraines, permanent brain damage and even death.
So when teams rush players back to the field from concussions early, it bothers concussion experts such as Michael Collins, who has served as a concussion consultant for the National Federations of High Schools and MLB, USA Rugby and the Pittsburgh Steelers. Collins recognizes a concussion as an energy crisis in the brain, which could lead to further potential effects.
“What we’ve learned is that during this energy crisis in the brain, don’t get hit in the head again,” Collins said. “There are a lot of potential effects of a concussion and it takes time to recover.”
But hits on the field aren’t the only issue; the recovery process presents problems, too. Ash didn’t just suit up and play Sept. 21 against Kansas State — he prepared all week. He watched video, studied plays and even went to class, all creating added stress on his brain.
“Because the brain is starved for energy, you don’t want to overtax it from an energy demand point,” Collins said. “One way to do this is working out and the other is school. Going to school and studying lengthens the time to recover from a concussion.”
Ash’s situation has brought the concussion prevention and management debate to the forefront in Austin. But doctors maintain concussion prevention more complicated than adding a few rules.
Locker said one of the biggest illusions centered around the concussion issue is the idea of the helmet being a safety regulation for concussions.
“The helmet cannot stop shaking the inside of the brain,” Locker said. “It’s a misnomer. Helmets are designed for skull fractures, not concussions.”
Locker said studies between old and new helmets find that better equipment doesn’t make a difference as long as it fits.
“It just has to feel good and fit,” Locker said. “If it comes off, the athlete is more vulnerable.”
Despite the advanced technology, the chance of injury is still there.
“It’s like an air bag in a car,” Locker said. “You can still die with the better technology.”
In fact, Locker believes that all the helmets do is encourage poor habits.
“No one tackles like they did in the ’70s,” Locker said. “They don’t tackle anymore. They just hit. If you take face masks off, they won’t hit anymore.”
That’s the biggest problem with concussion prevention — there is no way to stop the shaking of the brain. There’s no helmet for the brain; that’s the head’s job.
“You can’t stop the brain from shaking inside the skull,” Locker said. “If you can stop that, then you can prevent 97 percent of concussions.”
According to Collins, management is the key to aiding concussion recovery and preventing them from happening, and that starts with players and coaches.
“As someone who has been doing this for a long time, the biggest challenge I see is educating coaches on the basics,” Collins said. “What are the signs and symptoms? What decisions need to be made and how do I make those decisions? Once they are educated, they can really help the situation.”
Texas followed the NCAA Recommended Best Practices for a Concussion Management Plan for Ash’s injury, a set of guidelines for all NCAA institutions. With no clear NCAA protocol, this is more Texas’ process than the NCAA’s plan. It requires that student-athletes, coaches and other pertinent team personnel are educated annually on concussions.
Per Texas protocol, if a student-athlete sustains a mild head injury or exhibits signs of a concussion, he is immediately put through sideline screening by the athletic trainer. If he or she feels there is a positive finding for a concussion, Texas withholds the student-athlete from play for the rest of the day.
While much of the management up to this point has been monitoring behaviors and observing the athlete, the first measurable test has been created — the Immediate Post-Concussion Assessment and Cognitive Testing, or ImPACT test, which was co-founded by Collins.
“The reason we developed ImPACT was because there was never a way of measuring the injury,” Collins said. “The ‘how many fingers am I holding up’ and smelling salts were used not too long ago.”
The system does more than determine whether or not an athlete has a concussion — ImPACT helps further concussion research.
“We realized, how you can ever study, research or manage something without a way to measure it?” Collins said. “Then we decided to develop it on a computer so it would be repeatable and can measure reaction time and can be widely used.”
Before the first practice at Texas in baseball, basketball, diving, football, pole vaulting, soccer and softball, the medical staff issues a baseline test through ImPACT. A concussed student is considered “cured” when his original performance on the exam matches his post-concussion test.
But all of this testing can sometimes fail. When athletes come back too soon, it can cause long-term issues.
“If there’s anybody in the world with the best medical advice, it’s the University of Texas,” Locker said. “I’m not disclaiming that. It’s an inexact science. You just don’t know. Just because you had one and got well doesn’t mean you’re not going to get another one.”