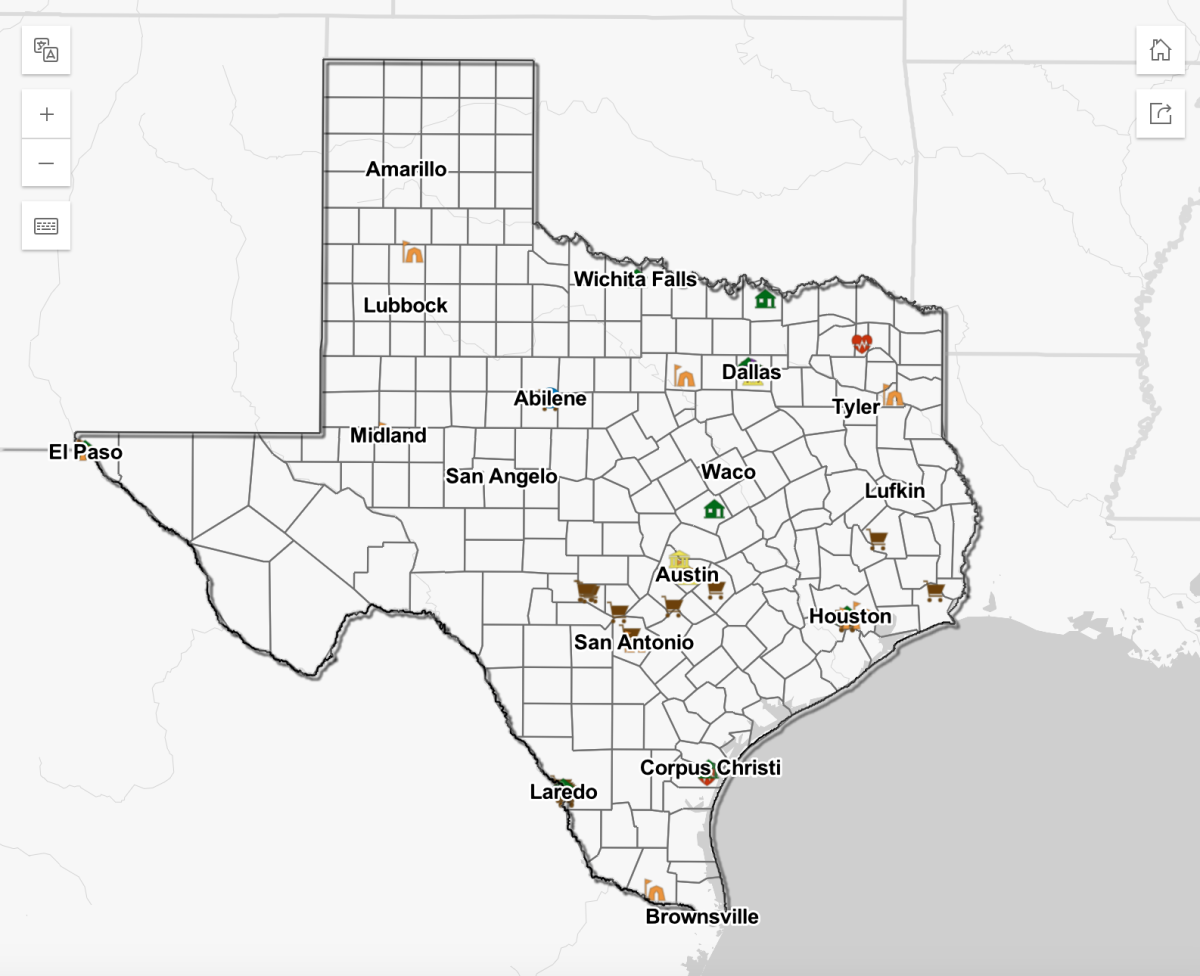
For medical professor David Lakey, getting his three daughters vaccinated for HPV, which causes 3 percent of all cancers in women and 2 percent in men, was a no-brainer. Yet, many in Texas remain unvaccinated, and according to a report lead by Lakey, the state ranks 47th in the nation for human papillomavirus vaccinations among adolescents.
“It challenges us to do better in protecting our kids from this type of disease,” said Lakey, UT System’s vice chancellor for health affairs and chief medical officer. “We are missing a tremendous opportunity to protect our kids.”
Conducted by the UT System, the study found that only Wyoming, Mississippi, South Carolina and Utah had worse adolescent HPV vaccinations rates than Texas. It’s important to get people vaccinated while they are young because their immune systems are much more receptive to the vaccinations, Lakey said. Before the age of 15, individuals only need two doses of the HPV vaccine six months apart, but after turning 15, they require three.
HPV has been directly linked to most cervical, anal, throat, neck and vaginal cancers along with 50 percent of vulvar cancers and 35 percent of penile cancers. The virus can be transmitted through kissing, close genital contact and sexual intercourse.
As of 2016, less than half of adolescents in the state had received at least one vaccination, and barely a third were up to date with their vaccinations, according to the report.
Administering the vaccine between the ages of 11 and 15 decreases the likelihood of the recipient already having been exposed to the virus, said Lois Ramondetta, oncologist and member of the Texas Medical Association’s HPV Task Force.
“No one wants to think about their kids being intimate with somebody, but (transmission of HPV) doesn’t even require intercourse,” Ramondetta said. “The earlier you (vaccinate), the less it’s even about relationships. It’s just about protecting you from future diseases that you might be able to get.”
Lakey said one of the main causes for the low-vaccination rate is misinformation about the HPV vaccine, which has only been in use for about 12 years. For years, Lakey said, people believed the vaccine was unsafe, but he said there is more than enough evidence supporting the vaccine’s safety and effectiveness.
In a press release that came out with the report, Divya Patel, assistant professor for population health at UT Health Northeast, said the best way to improve vaccination rates is to give the vaccines at the same time as other common childhood vaccines such as meningitis.
“If we can change attitudes and behaviors around the HPV vaccine and increase awareness that it is a cancer prevention vaccine, we can make a huge difference in people’s lives,” Patel said.
Ramondetta said physicians also need to make sure they do not isolate the vaccine when talking to parents and children about it. By making the vaccine seem more commonplace, it reduces the stigma and fear surrounding it, Ramondetta said.
“All I can do is continue to talk about it, continue to talk about the tragedy of diagnosing young girls with cervix cancer … and hope that people recognize that you never want to look back and feel like you missed an opportunity to protect your child or your patients,” Ramondetta said.