UT study records impact of pandemic on stigmatizing language around opioid use
May 3, 2022
The language used by health professionals when addressing opioid use on Twitter became increasingly stigmatized during the pandemic, according to a UT College of Liberal Arts study.
Scott Graham, a co-author of the study and associate professor of rhetoric and writing, said negative rhetoric about drug use has a negative impact on people’s ability to address and improve situations like the opioid epidemic. The study, published April 20, found that the use of destigmatizing language decreased during the pandemic in a reversal of previously recorded trends.
Graham said health professionals’ pandemic-related concerns could be responsible for the observed change.
“Health care providers are under tremendous stress right now because of the pandemic,” Graham said. “When you’re under stress like that, it’s harder to make really careful and conscious choices about your language. You slip back into default ways of talking, and unfortunately, speaking negatively about people who use drugs is a default way of talking in this country.“
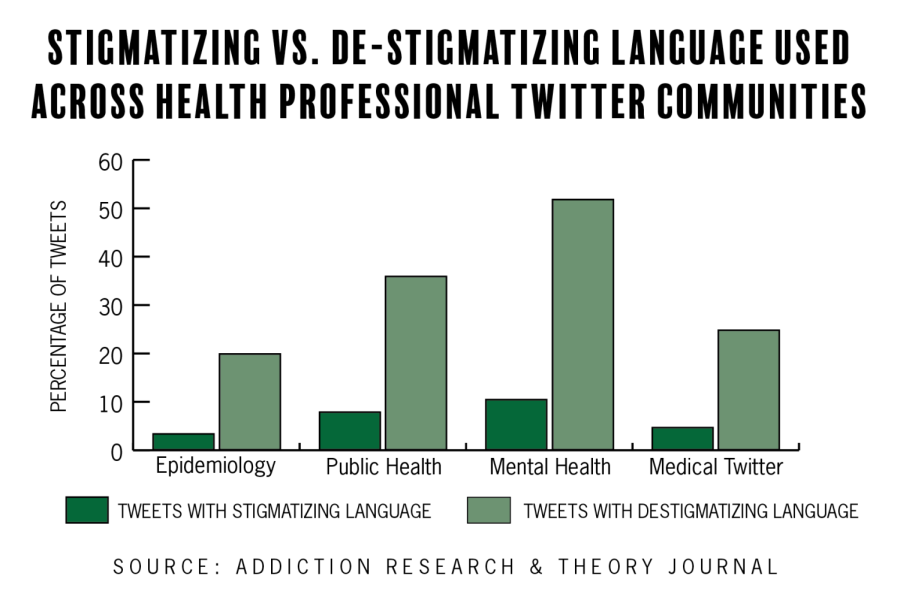
Using data from 2009 to 2021, researchers categorized tweets across multiple Twitter health communities as containing stigmatizing, destigmatizing or neutral language when addressing opioid use. Researchers found a trend of decreased condemning language until March 2020.
Kate Lower, director of the SHIFT program, which works to prevent and reduce substance misuse on campus, said person-first language is important when addressing misuse so a person’s disease isn’t seen as the entirety of their identity.
“It’s both for our understanding of that person and separating the disease from that person,” Lower said. “We are not our disease. We are not one thing and one thing only.”
Fiona Conway, co-author of the study and assistant professor of social work, said in an email that the impact of health care providers’ rhetoric is significant. People who misuse opioids and drugs may experience feelings of shame or guilt from their loved ones or the general public, and health professionals may act as a trusted source of compassion through information and care, she said.
“When health professionals use stigmatizing language on social media platforms like Twitter, the negative impact of their rhetoric is amplified,” Conway said. “People seeking care may no longer restrict their expectations of being shamed to specific individuals. They may feel like an entire profession is against them.”
Despite the reversal, Graham said tweets using destigmatized language still saw the most positive interactions, which will hopefully contribute to better language surrounding opioid use.
“If folks in those communities are intentional about rewarding good use of language about people who use drugs, then we’ll see more of it,” Graham said. “We can actually leverage the underlying functionality of Twitter to create better public health outcomes.”