UT researchers gain new insights into century-old multiple sclerosis modeling technique
November 15, 2022
UT researchers reexamined a long-standing model of multiple sclerosis in mice through a recently published study. The study compared multiple sclerosis itself with the model researchers use to understand the disease.
With additional information and genetic technology available in the modern age, biology junior Cara Fonken said it’s important to review the century-old model of research for multiple sclerosis and make sure it’s still effective.
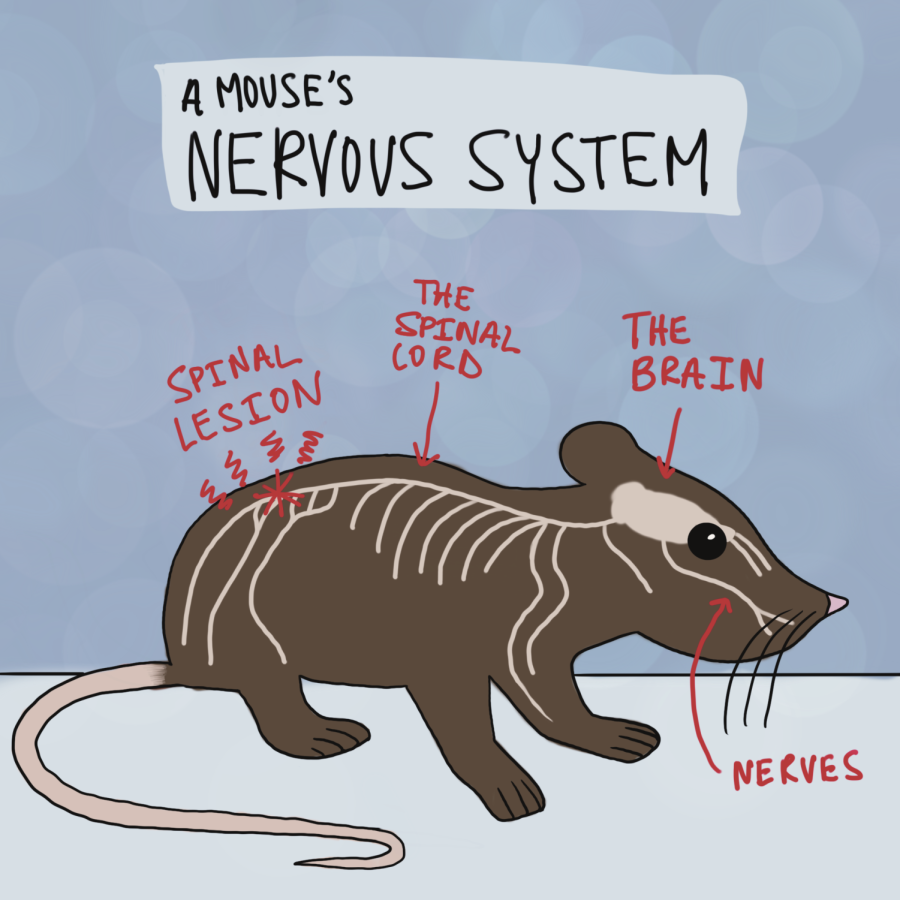
Experimental autoimmune encephalitis, or EAE, is an experimentally-induced condition in mice that mirrors the damage that occurs to human myelin sheath from multiple sclerosis, Fonken said. The myelin sheath is the outer coating of a neuron that allows signals to travel through the nervous system; when damaged, signaling is decreased or halted altogether. Researchers can induce EAE in mice in several ways. One method involves injecting mice with a naturally occurring peptide found in the myelin sheath along with another compound that stimulates an autoimmune response.
“Basically, it’s immunizing the animal against (itself),” Fonken said.
The study specifically focused on how EAE compares to multiple sclerosis in studies of the gut microbiome — microorganisms that support human digestive systems and have an influence on other regions of the body, including the brain.
Patients with multiple sclerosis have decreased biodiversity in their gut microbiome, so their immune systems aren’t as strong. “Some say that over 80% of the immune system is actually found in our gut,” neurology assistant professor Esther Melamed said. EAE has been used to fill in gaps in knowledge to understand better how gut microbiota affects the nervous system.
“The reason why we wanted to look specifically at the gut microbiome is because … (it has) a really important relationship in framing and in shaping our immune system,” Melamed said.
EAE has been the preferred way to model multiple sclerosis for over a century, but it’s not without its drawbacks, according to the study. Most notably, Fonken said that lesions stemming from EAE occur on the spine, whereas lesions from multiple sclerosis occur throughout a wider range of the nervous system, including the brain.
“There’s so many different symptoms (from multiple sclerosis) that can arise just depending on where lesions are located, and no one specifically knows where it originates,” said Jamie Palmer, a graduate student in the Institute for Neuroscience. “One of the issues is that everybody sort of induces (EAE) differently … there’s nothing yet that really fully encompasses all of the different symptoms of multiple sclerosis, which is difficult to do in an animal model.”
The opportunity to review a model that has been used for over a century allowed the researchers to compare its efficacy to newer modeling technology and receive more recent insights into the mechanisms of multiple sclerosis, Melamed said.
“I don’t think we’ll ever get rid of animals in research, likely because there’s a lot of knowledge that we can gain about the safety and efficacy of new medications, about mechanisms of disease that we frankly can’t do in humans,” Melamed said. “There are definitely important limitations to keep in mind in translating the studies, but I think it’ll continue with us.”