UT researchers recently analyzed the symptoms of long COVID and discovered a blood marker that differs in patients with fibromyalgia in comparison to long COVID, helping researchers contrast the two conditions.
Michael Brode, medical director of the Post-COVID-19 Program, said long COVID is typically defined as symptoms that last at least eight to 12 weeks after the initial infection and aren’t caused by another illness. According to the CDC, about 15% of adults in the US have had long COVID and about 5% currently have long COVID.
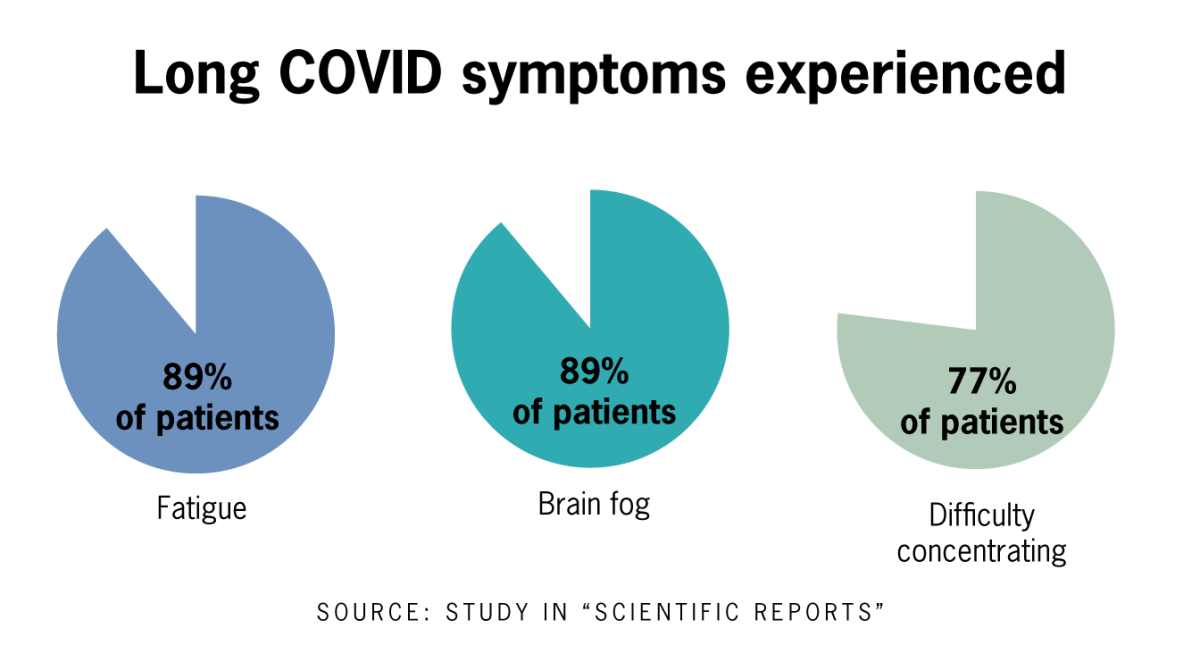
Brode said his team’s study showed the physical and mental health consequences of long COVID. The most common symptoms are chronic fatigue, brain fog and post-exertional malaise, Brode said. Additionally, untreated younger people had more neurological symptoms.
“Long COVID is this multi-system whole body disease,” Brode said. “It can be disabling; a lot of people lost their jobs, and a lot of depression, anxiety and mental health symptoms (were) associated (with long COVID).”
Brode said long COVID affects people of all ages and health levels, and clinics need to be established to adequately provide care for them.
“This is going to require intensive multidisciplinary clinics to meet all their different needs and make sure they have the social and mental health support to get on the road to recovery,” Brode said.
Kevin Hackshaw, associate professor in the department of internal medicine at Dell Medical School, said fibromyalgia, a musculoskeletal pain syndrome in which patients face pain and aches throughout their body, presents similarly to long COVID, in which patients have widespread aches and chronic fatigue.
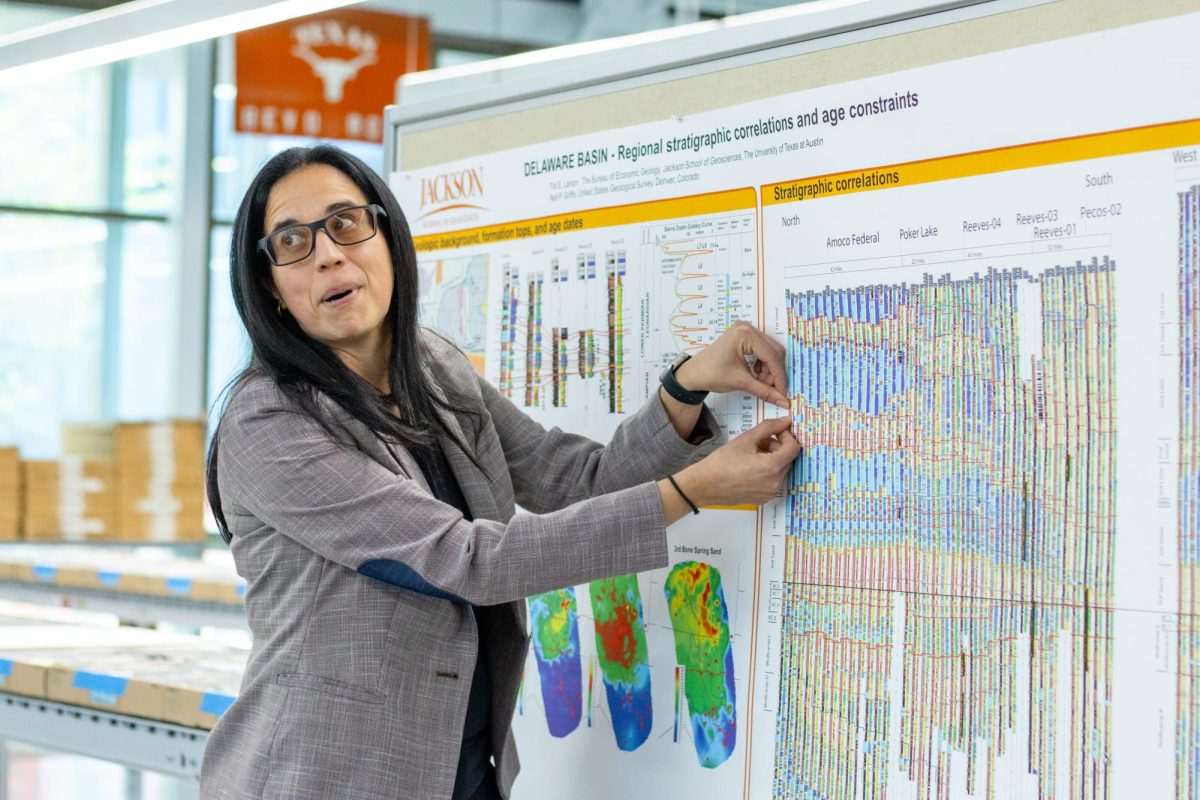
The researchers used a technology called vibrational spectroscopy that examines blood samples with a laser fitted to a computer. As the laser interacts with the molecules in the blood sample, observable changes occur and researchers can designate a vibrational “fingerprint” for each sample to classify them into different groups, Hackshaw said.
Hackshaw said he and his team studied 50 individuals with fibromyalgia and 50 individuals with long COVID and found a different “fingerprint” in those with fibromyalgia.
Hacksaw said the tests can be done with portable equipment at a patient’s bedside and are non-invasive, as they only require one-tenth of a teaspoon of blood from patients.
Hacksaw said the discovery of the molecular difference created more questions for the researchers to explore, including the possibility of targeting the marker that differentiates the two through therapeutics.
Hacksaw said while fibromyalgia affects 5% of the US population, scientists still don’t know the cause for the disease, but studying COVID-19 could lend insights into what causes fibromyalgia.
“Just the fact that we have two conditions that present clinically very similarly might give us some insight into the initiating etiology for fibromyalgia,” Hackshaw said.