UT researchers were selected for a grant from the National Institutes of Health for their antibody test to detect the virus that causes COVID-19.
Researchers will use the estimated $2.6 million grant over the next five years to study whether COVID-19 immunity will persist with age, said Gregory Ippolito, assistant professor of oncology and a lead researcher on the new test.
“It gives us a continued means by which to explore the human immune response to this virus,” Ippolito said. “Even though so much progress has been made, there’s still so much unknown and to be learned.”
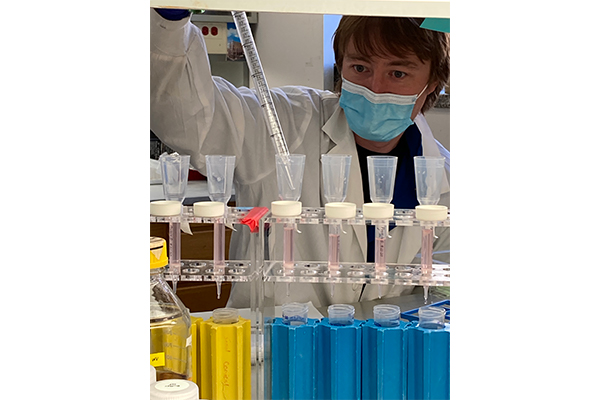
Ippolito and his colleagues at the Department of Molecular Biosciences created a more accurate antibody test to better determine if an individual had previously been infected with the SARS-CoV-2 virus that causes COVID-19.
“The antibody test we’ve developed is the gold standard certainly for scientific research,” Ippolito said.
Ippolito said the new tests are highly sensitive and quantify the number of antibodies a person has. He said the tests need a viral protein, which another research team led by chemistry associate professor Jason McLellan created.
“So, the first groups around the world who created antibody tests are the ones who already were producing the viral protein somehow inhouse,” Ippolito said.
Current antibody tests, known as lateral flow assays or LFAs, offer positive or negative results, whereas the new test is able to determine if a person has long-term immunity, Ippolito said.
“LFAs are like home pregnancy tests,” Ippolito said. “They can yield a lot of false negatives and also false positives.”
Carly Segura, a rhetoric and writing freshman, took a current antibody test and got binary results. She tested positive for antibodies and negative for COVID-19, meaning she had COVID-19 at some point, but there was no way to know when she contracted it or if she spread it to anyone.
“What worried me was the possibility that I could have spread it while I did necessary errands for my family,” Segura said.
Segura said the medical professional who administered her test told her she had “permanent immunity.” Segura said she still takes precautions to not contract or spread the virus.
“I know that I wouldn’t want my grandmother coming into contact with someone being careless, so why would I be careless knowing someone else may be just as vulnerable as her?” Segura said. “I hope other people carry that mentality, too.”
Editor’s note: This story has been corrected to reflect that researchers will use an estimated $2.6 million grant, not a $3.6 million grant, over the next five years to study whether COVID-19 immunity will persist with age. The Texan regrets this error.